
Angioplasty
Coronary angioplasty is also called percutaneous coronary intervention (PCI). It is a procedure very similar to Coronary Angiography (See HeartWest’s information leaflet) and is used to unblock narrowed sections of the coronary arteries. Just like angiography, small catheters are passed through either your wrist or groin into the heart and then balloons are used to widen any narrowing and stents are used to keep it from collapsing.

Why do it?
After performing Coronary Angiography, your cardiologist will recommend a coronary angioplasty procedure if needed in your particular circumstances. This usually means that Coronary Angiography has revealed narrowing in your coronary arteries, which can be treated, and the arteries unblocked by this procedure.
Most of the time people have angina and chest pains, which may get relieved after this procedure.
Coronary angioplasty can be done electively (as a planned procedure) or urgently in an emergency if there is a heart attack or some other cardiac emergency. A heart attack usually means that one of the coronary arteries on the heart is suddenly and completely blocked causing no blood flow down that artery, resulting in death of heart muscle tissue within a few hours unless the blood flow is restored by urgent coronary angioplasty.
What does coronary angioplasty treat?
Coronary angioplasty is a medical procedure used to treat blockages in the arteries of the heart, also known as coronary artery disease (CAD). CAD occurs when plaque (fatty deposits) builds up in the arteries that supply blood to the heart, reducing blood flow and causing chest pain or discomfort, shortness of breath, and other symptoms.
Coronary angioplasty is also often used as a treatment option for patients with stable angina, a type of chest pain that occurs during physical exertion or stress, in addition to acute coronary syndromes where arteries are acutely unstable and threaten to block.
What are the benefits of a coronary angioplasty?
Improved blood flow to the heart
The primary benefit of coronary angioplasty is that it can restore blood flow to the heart by opening up blocked arteries. This can help alleviate symptoms of CAD, such as chest pain or discomfort, shortness of breath, and fatigue.
Reduced risk of heart attack
By restoring blood flow to the heart, coronary angioplasty can also help reduce the risk of heart attack, particularly in patients with unstable angina or acute coronary syndrome.
Improved quality of life
CAD can have a significant impact on a patient’s quality of life, limiting their ability to perform daily activities and causing ongoing symptoms. By improving blood flow to the heart, coronary angioplasty can help improve a patient’s overall quality of life.
Lower healthcare costs
In some cases, undergoing coronary angioplasty may be less expensive than other treatment options for CAD, such as bypass surgery. Additionally, because angioplasty is a minimally invasive procedure, it may result in shorter hospital stays and a quicker recovery time compared to other treatment options.
Before the procedure
Coronary Angioplasty / PCI is performed by Interventional Cardiologists. It’s done in a hospital in a special operating room called Catheterization Laboratory (Cath Lab). You will make the decision to go ahead with Coronary Angioplasty / PCI in consultation with your cardiologist. He/she will explain the procedure and will get you to sign a consent form. Please make sure you ask any questions that you may have before you sign the consent. Occasionally the procedure is explained much earlier while consent is signed just before the procedure, which allows you to have time to think about it and ask questions.
Before you come to the hospital, you may be asked to have other tests like blood tests, an electrocardiogram (ECG), and a chest X-ray.
You may be admitted to hospital the night before your Coronary Angioplasty / PCI, but most people are admitted the same day, usually two hours before the procedure. In most instances, patients will be discharged from hospital on the next day, staying in CCU overnight. You will not be allowed to drive back, so there should be arrangements for your transport back home.
You will be asked not to have anything to eat or drink for at least six hours prior to the procedure.
Once you arrive in the hospital, you will be greeted by the hospital staff and then given a bed. You may be asked to remove any jewellery that you might be wearing and to put on a hospital gown. You will be shaved in the area where the catheter will be inserted. An intravenous (iv) line will be inserted to administer IV fluids / medications as needed.
How safe is a coronary angioplasty?
Coronary angioplasty is generally considered to be a safe procedure, although as with any medical procedure, there are some risks involved. The overall risk of these complications is relatively low. The exact risk of complications will depend on factors such as the patient’s age, overall health, and the complexity of the procedure. In general, the risk of complications is higher in older patients, those with other underlying health conditions, and those who require more complex procedures.
As Coronary Angioplasty / PCI is an invasive procedure, there are some risks. Your Cardiologist will explain these. However serious problems are uncommon. Most people have no trouble, and the benefits usually far outweigh the risks. You are encouraged to discuss these with your cardiologist and get clarification about any concerns that you may have about Coronary Angioplasty / PCI.
Common coronary angioplasty risks include:
- Bleeding or bruising at the site of the catheter insertion
- Infection
- Damage to blood vessels or organs
- Allergic reaction to the contrast dye used during the procedure
- Blood clots
- Stroke or heart attack
- Restenosis, which is the re-narrowing of the treated artery
Patients can take steps to reduce their risk of complications by following all pre- and post-procedure instructions, including taking any prescribed medications and avoiding strenuous activity for a period of time after the procedure.
It’s also important to attend all follow-up appointments to monitor the success of the procedure and address any potential complications that may arise.
What happens during a coronary angioplasty procedure?
Just like Coronary angiography, Coronary Angioplasty / PCI is also done in special catheterization laboratories (‘Cath-Labs’) that look like operating theatres. The procedure involves X-Rays and injecting a special dye containing iodine into the blood vessels. You may feel hot when this dye is injected.
You will be taken to the Cath Lab and asked to lie on a narrow table, which can be moved in all directions during the test. You will be connected to a few monitoring devices and then the shaved parts (either your wrist, groin or both) will be cleaned and sterilized with a special solution (which may feel cold). After that your whole body will be covered with sterile drapes.
You will be given mild sedation through intravenous drip to help you relax. Your cardiologist will then inject local anaesthetic into your wrist, arm or groin from where the catheter is to be inserted. A sheath will then be inserted into the artery at that point. Through this sheath, various catheters, wires and instruments will be inserted and advanced to reach the heart and changed as required. Different catheters / wires / balloons and stents are used as needed to unblock the arteries as required. There is an X-Ray camera that moves around and records short movie clips of what the interventional cardiologist is doing inside your heart. Most people do not feel any pain or sensation during the procedure. There are no nerves inside your arteries, so you will not feel the movement of catheters or wires through your body. Some people have nausea or chest discomfort when the dye is injected, or when the balloon is inflated (for the balloon angioplasty), but this does not last long.
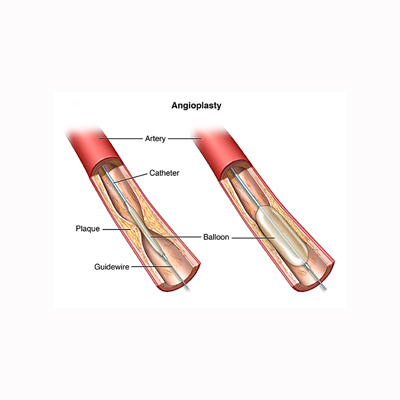
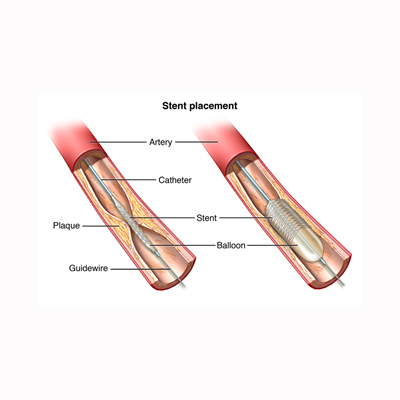
When a narrowing which needs to be treated is identified, an extremely thin wire is then passed through this narrowing to lie beyond this narrowed area. On this wire a special collapsed balloon is then advanced and placed accurately within the narrowing. The balloon is then inflated causing the narrowed part to become wider. The balloon is then deflated and withdrawn but the wire stays. This is usually followed by advancing another special collapsed balloon, which has a metal stent on it. The stent is a metal mesh, which can expand to a predetermined size as the balloon is inflated. Again this is placed within the narrowed part and the balloon is inflated. The stent expands and widens the artery. The balloon is then deflated and withdrawn leaving the stent embedded inside the artery. Once the stent placement is deployed, the stent cannot be moved again. Deployment is seen, confirmed and documented via the X-Ray clips recorded intermittently throughout the procedure.
If there are more blockages, the same procedure is repeated to insert additional stents if needed. If there are many blockages, then the procedure will have to be repeated after a few days / weeks as the total dose of dye used and radiation involved can be too much for one sitting.
Total time taken for the procedure varies depending upon how many blockages are tackled and how complex and time consuming they are. Hence there is no accurate time prediction beforehand.
What happens after the procedure?
When the procedure is finished you will be taken to CCU and your heart monitored continuously for the next 24 hrs. The sheath through which the procedure was done may still be in your groin, which may be removed a few hours later depending upon some blood results. After the sheath is pulled out, your groin will be pressed for about 10 minutes to stop bleeding.
Bleeding from the procedure site can happen later as well. For this reason you will be given specific instructions on how to look after the area, what to avoid and what to look for.
If your heart is stable after 24 hrs you will be discharged home.
You should avoid any heavy activities such as lifting or straining for about a week until the small wound has healed.
You should not drive a car for one week after having an angioplasty / PCI unless permitted by your cardiologist. If you have a heavy / commercial vehicle licence, you should check with your cardiologist regarding going back to driving as per rules laid by the Australian government.
You may get a bruise from where the procedure was performed. This is not serious but it may be slightly painful for a few days.
What is a coronary artery bypass?
In some cases, coronary artery bypass surgery may be recommended after a failed or complicated angioplasty procedure. For example, if the artery being treated with angioplasty becomes completely blocked or if complications such as significant bleeding occur, a bypass surgery may be necessary to restore blood flow to the heart. However, in many cases, angioplasty can successfully treat blockages in the coronary arteries, and bypass surgery is not necessary.
A coronary artery bypass is a surgical procedure that’s performed to treat significant blockages in the coronary arteries, which supply blood to the heart muscle. During the procedure, a surgeon creates a new pathway for blood to flow around the blockage, typically by taking a blood vessel from another part of the body and grafting it onto the affected artery.
Coronary artery bypass surgery is generally reserved for cases where the blockages are severe and angioplasty is not feasible or not likely to be successful. It’s a more invasive procedure than angioplasty and requires a longer recovery time, but it can be very effective in improving blood flow to the heart muscle and reducing symptoms of coronary artery disease.
Where can I go to find out more about a coronary angioplasty procedure in Melbourne?
HeartWest is the largest cardiology group in the western and northwestern corridors of Melbourne, with 4 major locations and 3 satellite sites.
At HeartWest, our qualified experts will provide you with the best cardiology care. You will experience nothing but professionalism, care and courtesy; from your first interaction with our staff, to going through tests, procedures and consultations.
- Our cardiologists have expertise in all fields of adult cardiology, including;
- General cardiology
- Heart failure
- Cardiac imaging (including stress echocardiography)
- Interventional cardiology
- Electrophysiology & pacing
- Cardiothoracic surgery
Contact us for efficient and affordable specialist heart care services
